Written by Anneri Fourie | Crises Control Executive
When A Well Practised Plan Meets A Real Incident
An emergency response plan can look flawless in a boardroom. Staff know the steps. Exercises run smoothly. Everyone leaves the drill confident that the organisation is prepared.
Then a real incident happens, and the same team that performed so well in rehearsal suddenly struggles to stay aligned.
Phones start ringing. Teams begin acting on partial information. Leaders ask for updates that nobody can fully answer. Staff hesitate because they are unsure who is leading the response.
The gap between planning and reality becomes visible within minutes.
This is not a failure of training or professionalism. It is a structural gap between knowing what should happen and having the systems in place to make it happen under pressure.
The organisations that handle real incidents well are not necessarily the ones with the most detailed plans. They are the ones that have translated their emergency response plan into something operational, something that guides action rather than relying on memory.
This article explores why drills often fail to reflect real conditions, what actually happens during live incidents, and how hospitals are moving from procedural readiness to operational readiness through structured coordination.
What An Emergency Response Plan Really Means
An emergency response plan is a framework that defines how an organisation detects incidents, escalates concerns, communicates across teams, and coordinates actions to maintain safe operations.
On paper, this often looks clear and logical. Roles are defined. Escalation pathways are mapped. Communication channels are listed.
In practice, the real value of a plan lies in how easily it can be activated when information is incomplete and pressure is high.
If staff have to interpret procedures while managing an unfolding situation, response becomes inconsistent. If the plan is operationalised through structured workflows, it becomes a guide that supports decision making in real time.
A Realistic Scenario Hospitals Will Recognise
Picture a large hospital on a busy weekday morning.
A monitoring system flags irregular activity within a clinical platform. At first the issue seems minor. Within minutes, clinicians notice delays accessing patient information. Call queues begin to grow.
At the same time, facilities teams receive an alert from a storage area where temperatures have moved outside acceptable limits. Elsewhere, a clinical team is assessing whether a patient safety concern requires escalation.
Each situation is manageable on its own. The difficulty emerges when they overlap.
Senior leaders need a clear view of what is happening. Clinical teams need direction. IT needs to investigate. Operations must keep services running.
Communication begins quickly, but not in a coordinated way. Updates are shared through phone calls, messages, and quick conversations in corridors.
Within half an hour, people are working hard, yet nobody has a complete picture.
The Operational Pressure Created By Real Incidents
Live incidents rarely unfold in a controlled sequence. Information arrives in fragments. Priorities compete. Teams must act while still trying to understand the situation.
Under these conditions, staff rely on familiar habits such as calling colleagues or sending quick updates. These behaviours feel natural and reassuring, yet they can create different versions of the same situation across departments.
Without a shared structure, the organisation loses situational awareness.
This is the moment where the difference between having a plan and having operational readiness becomes clear.
Communication And Coordination Challenges
During the scenario above, communication is constant. People are engaged and responsive. The difficulty lies in coordination.
Common issues begin to appear:
- Different teams receive different information
- Leadership receives updates without context
- Staff are unsure who owns which tasks
- Actions are duplicated or delayed
- Documentation begins after the fact
These challenges are rarely caused by poor performance. They reflect systems that depend on individuals to coordinate rather than providing coordination as part of the workflow.
Where Traditional Approaches Struggle
Many hospitals still rely on manual escalation methods. These approaches depend on experience and professional judgement, both of which are valuable.
The limitation appears when incidents become complex.
Phone calls reach individuals but not teams. Emails provide written records but do not confirm action. Messaging platforms share updates but rarely assign responsibility.
After the incident, teams often try to rebuild timelines from memory, which makes it harder to understand what actually happened and what should change.
This is not a failure of planning. It is a limitation of tools that were designed for everyday communication rather than coordinated incident response.
Why Drills Do Not Fully Prepare Teams For Reality
Exercises are essential. They build confidence and familiarity with procedures.
Yet drills usually occur in controlled conditions with clear starting points and defined scope. Real incidents develop gradually, overlap with other demands, and present incomplete information.
Without systems that mirror training in real time, organisations often find that strong exercise performance does not guarantee consistent live response.
Most organisations do not have a planning problem. They have an execution gap.
The Structured Response Approach
A structured approach connects communication, roles, and actions through defined workflows.
When an issue is detected, the relevant plan is activated quickly. Alerts reach the right people based on their roles. Tasks are assigned with clear ownership. Updates are shared through a central channel that provides leadership with visibility.
Incident management software supports this by turning static plans into operational processes.
Rather than relying on individuals to interpret procedures, the workflow guides the response, helping teams stay aligned even as conditions evolve.
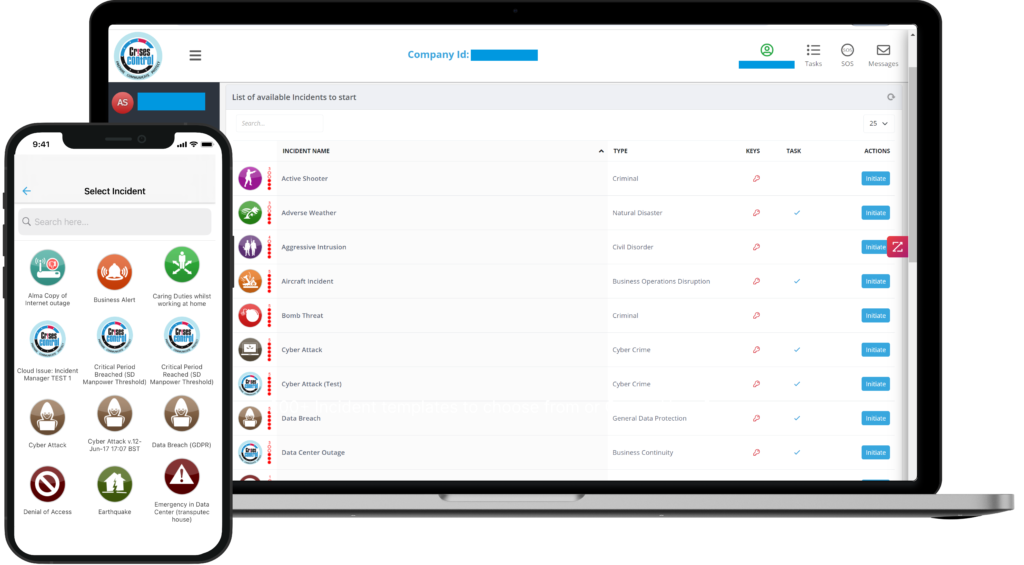
Interested in our Incident Management Software?
Flexible Incident Management Software to keep you connected and in control.
How Hospitals Are Operationalising Their Plans
Healthcare organisations are increasingly embedding their response processes into digital platforms.
In practice this means:
- Linking escalation workflows to clinical and operational systems
- Using triggers to detect issues early
- Assigning tasks automatically based on roles
- Providing real time visibility for leadership
- Capturing a complete record of actions
Platforms such as Crises Control support this approach by digitalising plans and enabling structured activation across departments.
For example, rapid response workflows can be triggered from fixed devices or mobile applications. Operational alerts can notify teams when thresholds are breached. Communication remains consistent even outside normal hours.
The objective is consistency rather than automation for its own sake.
The Human Element Of Decision Making
Healthcare professionals make judgement calls constantly. No system replaces that expertise.
What structured coordination does is reduce the mental effort required to understand who is doing what and whether the right people have been informed.
When staff trust the coordination layer, they can focus their attention on clinical and operational decisions rather than trying to piece together the situation.
This supports confidence without removing professional judgement.
Governance And Accountability
Hospitals must demonstrate how incidents are managed and how decisions are made.
Manual processes make this difficult because timelines are often reconstructed afterwards. Gaps are common, which makes learning harder.
Digital coordination creates a real time record of alerts, acknowledgements, and actions. This strengthens governance and supports continuous improvement by providing a clear account of events.
Lessons From Real Operational Situations
Live incidents consistently highlight the same lessons.
Plans must be simple to activate. Communication must be structured. Roles must be clear. Visibility across departments supports coordination. Documentation should occur during the response rather than afterwards.
Organisations that address these areas are better positioned to manage complex situations without losing situational awareness.
Moving From Planning To Operational Readiness
An emergency response plan is only effective when it guides action during uncertainty.
The shift from documented procedures to operational readiness requires tools and processes that connect detection, communication, and coordination.
Hospitals that operationalise their plans create a shared foundation for decision making. Teams remain aligned, leadership maintains visibility, and response becomes more predictable even when events are complex.
Crises Control provides a practical example of how structured workflows, role based communication, and cloud access support this transition by ensuring plans are accessible and actionable across the organisation.
Final Thoughts
The gap between drills and real incidents is not about capability. It reflects the difference between practising a scenario and managing an evolving situation with competing demands.
Organisations that translate their emergency response plan into operational workflows create the conditions for clearer communication, stronger coordination, and improved oversight.
For leaders reviewing their approach, the key question is whether response depends on memory and informal communication or is supported by structured systems that guide action.
Request a FREE Demo