Written by Anneri Fourie | Crises Control Executive
SOS panic button App hesitation in hospitals is rarely about technology. It is about human judgement under pressure.
When something feels wrong in a hospital, the first reaction is rarely technical. It is human.
A nurse notices a patient deteriorating faster than expected. A clinician senses tension building in a waiting area. A staff member feels unsafe during a late shift. In these moments, the decision to escalate is immediate in theory but often slower in practice.
The problem is not a lack of professionalism or care. It is uncertainty.
Uncertainty about whether the situation meets the threshold.
Uncertainty about whether escalation will disrupt others unnecessarily.
Uncertainty about whether pressing the button will lead to clear action.
That hesitation creates a gap between recognising risk and activating response.
The solution is not simply providing an alert mechanism. It is creating a clear, trusted pathway that makes escalation feel supported, structured, and appropriate.
This article explores why hesitation occurs in clinical environments, what organisations often overlook, and how structured activation supported by clear ownership and communication helps teams act with confidence.
What Is An SOS Panic Button App In Healthcare
An SOS panic button App is a digital tool that allows healthcare staff to trigger an incident alert instantly, notifying the appropriate teams and activating predefined response workflows.
In practice, it connects frontline staff with an incident management platform with SOS alerts so escalation is visible, coordinated, and documented from the first moment.
It is not simply a notification feature. It is a structured activation pathway that links recognition to coordinated response.
When implemented well, it removes ambiguity and gives staff confidence that escalation is both appropriate and supported.
Why Hesitation Exists In Clinical Environments
Healthcare professionals make judgement calls constantly. Deciding when to escalate is rarely straightforward.
Even experienced staff can hesitate for understandable reasons.
Fear Of Overreacting
Staff often worry about escalating unnecessarily. In busy environments where teams are managing competing priorities, no one wants to create disruption without justification.
Lack Of Clear Thresholds
When activation criteria are unclear, staff rely on personal judgement. This leads to inconsistency across departments and shifts.
Previous Experiences
If past escalations resulted in confusion or criticism, confidence decreases. Staff may delay activation while seeking reassurance.
Informal Escalation Culture
In some organisations, escalation still depends on verbal confirmation. This introduces delay even when instincts are correct.
These factors combine to create behavioural friction that slows response even when people recognise risk early.
A Real Scenario Many Organisations Recognise
A nurse notices that a patient’s condition is deteriorating unexpectedly. She considers activating an alert but pauses to confirm with a colleague. The colleague suggests monitoring for a few more minutes.
Those few minutes pass before escalation occurs.
The delay is not caused by lack of awareness. It comes from uncertainty about whether activation is appropriate and what will happen next.
Situations like this happen daily across healthcare environments. The lesson is clear. Escalation must feel simple and supported if organisations want consistent response.
The Real World Impact Of Delayed Activation
Delayed escalation affects more than speed. It affects coordination and visibility.
When incidents are not declared early, organisations often experience fragmented communication and parallel decision making. Leadership gains awareness later than they should. Documentation begins after the fact rather than in real time.
These challenges increase operational risk and make learning from incidents more difficult.
Strong activation pathways reduce this gap by ensuring response begins with structure rather than informal coordination.
The Myth That Training Alone Solves Hesitation
Many organisations invest heavily in drills and simulations. Training builds awareness and skill, but it does not remove uncertainty on its own.
In real environments, pressure, workload, and competing priorities influence behaviour. Staff often revert to familiar habits, especially when escalation pathways are not simple or visible.
Systems that mirror training workflows during live incidents reinforce consistency and reduce hesitation.
How A Clear Activation Pathway Changes Behaviour
When escalation becomes straightforward, confidence increases.
A hospital staff emergency alert system that provides one touch activation aligned with clinical protocols allows staff to act without second guessing.
Clear pathways reduce cognitive load because staff do not need to interpret thresholds under pressure. Leaders gain early visibility, ownership is defined immediately, and teams move from recognition to coordinated response more quickly.
Behaviour changes when people trust the process.
Manual Escalation Versus Structured Digital Activation
Manual escalation often relies on phone calls, overhead paging, or messaging. These methods depend heavily on memory and availability.
Structured activation through incident management software creates a different experience.
Manual methods often lead to delayed escalation, fragmented communication, and limited documentation. Structured activation allows incidents to be declared quickly, roles assigned automatically, and situational awareness shared across departments.
The difference is clarity rather than technology alone.
Behavioural Design Matters More Than Features
Organisations often evaluate systems based on functionality. Behavioural design plays an equally important role.
An SOS panic button for healthcare staff must feel intuitive and aligned with daily workflows. If activation requires multiple steps or unclear choices, hesitation increases.
When activation is simple, visible, and supported by clear ownership, staff feel confident using it.
Tools influence behaviour only when supported by process design.
The Role Of Communication In Early Escalation
Escalation without communication structure can create confusion.
An effective crisis alerting system ensures alerts reach the right people with clear context. Structured communication provides role specific notifications, confirmation of receipt, and consistent updates.
This reduces uncertainty and improves coordination across departments.
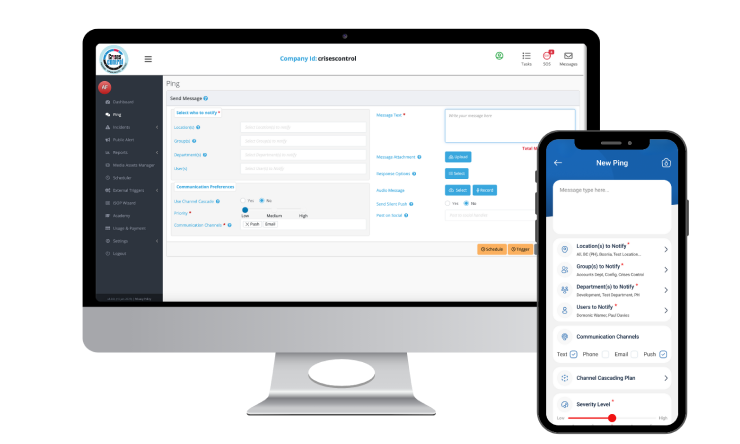
Interested in our Ping Mass Notification Software?
Efficiently alert everyone in seconds at scale with our Mass Notification Software.
Operational Pressure And Human Factors
Hospitals operate under constant pressure. High patient volumes, staffing challenges, and competing priorities shape decision making.
Under pressure, teams revert to familiar behaviours. If escalation relies on informal communication, variability increases.
Structured emergency communication solutions provide consistency by embedding escalation logic into workflow so response remains disciplined even during demanding conditions.
How Crises Control Supports Confident Escalation
Healthcare organisations are increasingly adopting platforms that embed structured activation into everyday workflows.
Crises Control supports this approach by digitalising response plans and providing role based incident activation, reliable communication, and cloud access during disruptions.
By reinforcing ownership and visibility, it helps organisations ensure escalation remains consistent even when teams are under pressure or geographically dispersed.
What Leaders Should Evaluate
Leaders reviewing their escalation approach should consider how easily staff can trigger incidents, whether ownership is assigned immediately, and whether communication is traceable.
They should also assess whether workflows support consistent response and whether documentation is captured automatically.
If escalation depends on informal coordination, hesitation will remain.
Creating Confidence In Escalation Decisions
Reducing hesitation is not about encouraging more alerts. It is about creating confidence that escalation is appropriate and supported.
When staff trust the pathway, they act decisively. When processes feel uncertain, hesitation fills the gap.
A well designed SOS panic button App supported by clear workflows allows organisations to move from uncertainty to coordinated response with confidence.
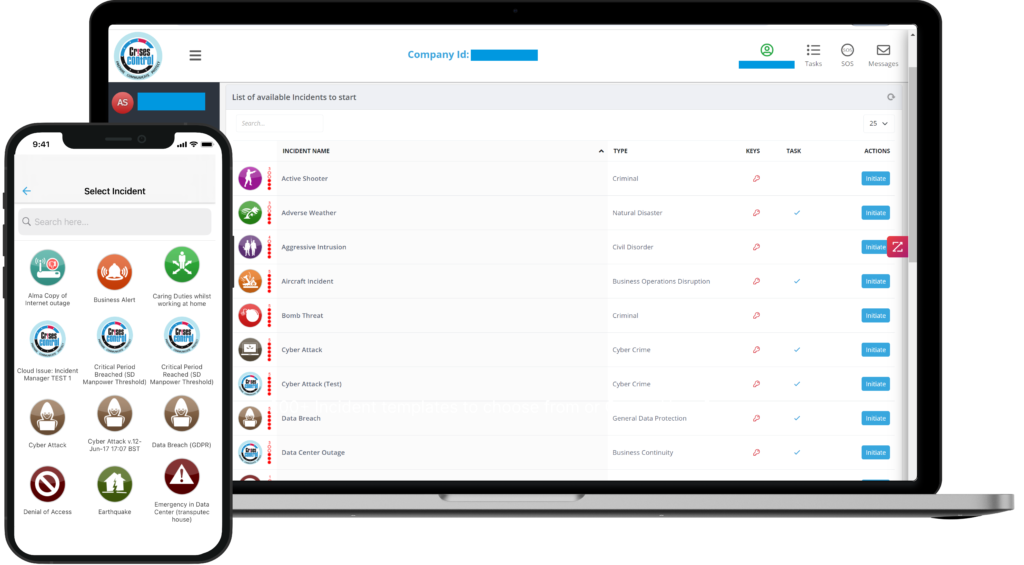
Interested in our Incident Management Software?
Flexible Incident Management Software to keep you connected and in control.
Conclusion
Healthcare environments demand both speed and judgement. The challenge is not simply recognising incidents. It is ensuring escalation pathways support staff in acting with confidence.
When activation is structured, teams respond with clarity, leadership gains visibility earlier, and coordination improves across departments.
Organisations using platforms such as Crises Control are increasingly embedding structured escalation into daily operations to reduce hesitation and strengthen response.
If you are reviewing your current approach, consider whether escalation feels simple and supported or uncertain and informal.
Request a FREE Demo

